cw: cancer
Waiting on Radiation & Occupational Therapy Begins
It has now been over 5 weeks since my last surgery (and 8 weeks since the first). The waiting time in between action on the breast cancer is so tedious. In the first 3 weeks, I wasn't supposed to lift my arm above 45 degrees, so that the plastic surgery stuff connecting my lymph channels and veins could heal well. Last week I started Occupational Therapy (OT) at the Lymphedema clinic in Yakima.
 |
| chart of the lymphatic system in the lymphedema clinic |
The goal of OT is to help me learn how to prevent myself from getting lymphedema, since I'm more at risk of getting it after the ALND surgery. I don't have it now, though the OT doctor seemed to suggest that maybe I have 0 level lymphedema, which means no swelling. I don't see how that's different from not having it. Though I like my Occupational Therapist, I'm not sure we are 100% sympatico in our communications. Several times in our first appointment she asked me to move my arm a certain way, then laughed at me when I had no idea what she was asking for.
 |
| Sean is painting the dining room, so he laid down a tarp (flat) and the cats have been frantically attacking the phantoms underneath it |
The first appointment appeared to be mostly to take measurements of my arms and back, to test how much I could move the arm, check the scar(s), and teach me some basics about lymphedema and prevention. The instructions from plastic surgery were to avoid lifting above 45 degrees in the first 3 weeks, but they didn't give me much guidance about what to do after 3 weeks. I've been doing the arm exercises, but only one of the 10 had me move the arm above 45--and that was only to 90 degrees.
 |
| The first day they were too terrified to walk through the room, but this morning their hunting instincts were cranked up |
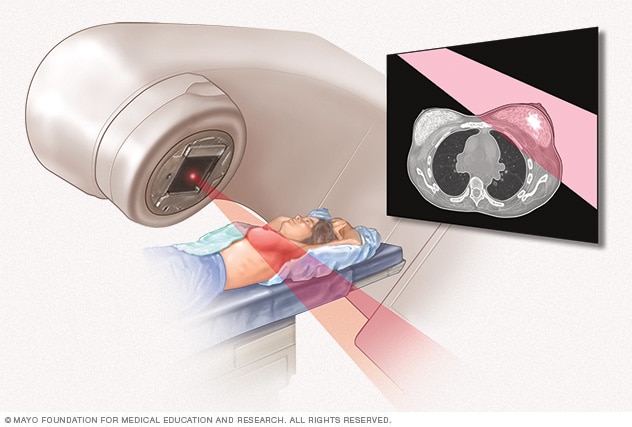
The upshot was that I hadn't tried to get my arm all the way above my head until I was at the lymphedema clinic (under supervision was my thought--I didn't want to ruin the work of the plastic surgeon). I can't start radiation until I can get it comfortably above my head for the CT, so the second goal of OT has been to achieve that position.
 |
| "I am a fierce tiger" |
With that in mind, I had a second OT appointment they day after the first (added at last minute to try to speed up my access to radiation). The second appointement was very different. She pulled on my shoulder and stretched my arm in all sorts of ways, put pressure on my scar and generally made the arm feel better and worse simultaneously. Then we went into the gym (the clinic has its own gym for OT/PT) and she had me do a bunch of exercises like climbing the "finger ladder" (which is an actual wooden ladder-like thing on the wall), and lifting and rolling a variety of balls and sticks to move my arm.
 |
| (see how fierce?) |
My homework was just to do these three sets of exercises twice a day. I've been doing them (and a bit more in the form of housework), but I still feel like I've got a ways to go. My OT said that I'd probably be ready for radiation prep this week, but I'm not so sure. As of today, I do not think I can get the arm fully overhead unless there's going to be more propping up than I anticipate. I do have another OT appointment tomorrow, so I hope she'll help me understand.
 |
| the battle is ready to begin |
Other than the OT, I've been doing a whole lot of nothing during the past 5-8 weeks. I know my body has been healing, but I'm pretty impatient and not being "supposed" to do stuff around the house has gotten old. It was kind of nice that, when Sean moved furniture out of the dining room (he's starting to repaint it), I wasn't asked to help, but I'm also not able to spend much time in the studio without getting a pretty serious backache.
 |
| I started glazing a bit after my first surgery, but it wore me out. Coming back to it (in small doses) weeks later means I can't remember how many layers I'd already done, or what the color plan was going to be! |
Reading About Breast Cancer, Again
Because I can't do much physically, and because I am not actively in treatment (or hadn't been until OT started last week), I finally got back to reading about breast cancer. I had set aside the reading early on during chemo because it was stressing me out. I was getting scared and worried about treatment and the unknowns of the whole experience.
 |
Dr. Susan Love's Breast Book, 6th Edition (2015)
|
Some friends had loaned me Dr. Susan Love's Breast Book and I had read a bit, but had to stop. I always wanted to get back to it, but I felt I had to wait until I was mentally ready. So over the past weeks I read almost the whole thing.
 |
can you feel the tension?
|
I read nearly every page of the first 505 pages of the book, but came to a screeching halt at the last section "Recurrence of Breast Cancer." I closed the book for a few days while I decided whether I was mentally ready to think about cancer coming back. I decided that I could proceed with caution and skimmed a bit of the first chapter (chapter 19), but decided not to read on. Hopefully I will never have to think about this stuff, and at this point I think knowing just enough to monitor my health appropriately "is indicated" for my situation. As my husband accidentally pointed out last night, I'm not even done with the first round!
 |
the battle commences
|
Writing as a way of processing information
I read this book a lot differently than one might read a general interest book, as you can see by the many tabs in my (borrowed) copy. And, as I've been doing all along, I process this information by writing about it. So, I guess what follows is a (long and personally skewed) book review that is intertwined with my own experiences of the thing that caught my attention in the book. I'm sharing it publicly for three reasons:
- Someone in a similar situation might find this information useful
- I sometimes look back at posts to know what I was thinking/doing at the time
- My family/friends might be interested
But if you are just following along for updates about how I'm doing, that stuff mostly ended in the first section, so feel free to stop now (or just look at the cat pictures ;-). On the other hand, I
Dr. Susan Love's Breast Book, 6th Edition (2015)
First, this book is sometimes referred to as the "bible" of breast cancer, so you know it's pretty reliable. It's also super thick (690 pages, including the notes and index) and chock a block with information about breast health, cancer development, treatment, and more. It's also the 6th edition, and the author writes about things that have changed since the first or the fifth edition and things she's added based on feedback on the earlier editions.
 |
| fight! |
But, it is also fairly old by now (and my understanding is the author does not plan to revise it). I read somewhere, earlier in this process, that you shouldn't rely on any book published more than 7 years ago. I did notice a few places where the standards have clearly changed over that time (I think I point out a few instances below), but I do wonder how much of the rest of this is now out of date. I don't have an answer, but is probalby good to keep in mind when reading the book or my discussion/review.
 |
| just two lumps with tails |
Additionally, one more caveat: I have read a lot about breast cancer over the past 8 months, so things that strike me are (probably) mostly things I haven't already internalized or things that I haven't already discussed here. If I do repeat myself, it's probably because I haven't fully processed the information (or because my chemo brain made me forget ;-).
Screening
The first thing that caught my attention was these two graphs on page 154 of the Screening chapter (chapter 7). They both start with a group of 200 women who do or do not get cancer screenings. This is for women age 50-70 and the screening happens every 3 years. For those of us over 40 and under 50, there often has appeared to be a gap in statistics or information, not just in Love's book. In fact, screening guidelines still vary for this population (i.e. me last year!).
 |
chart comparing the results of screening over 3 years (page 154)
|
In the first, of those 200 women who were not screened, 12 are diagnosed and treated and 4 die. In the second, of those 200 screened, 15 are diagnosed and treated, 3 die, and 3 are over-treated. So the trade-off is that those who were screened see one fewer death, but also 3 people are overtreated. My husband asked if those who are overtreated might die from their treatments, but it doesn't say. What frustrates me about this comparison is that it includes only one type of pain and trauma as a "negative." In this comparison, the pain and trauma of folks who are over-treated (meaning folks who go through surgery, radiation, and/or chemotherapy for a cancer that never would have progressed to a dangerous level) is acknowledged, but not the pain and trauma of folks for whom the disease was caught late and had to go through more treatment that they would have if the disease had been caught earlier with mammography screening.
 |
| reconsidering their positions |
Of course this means me and that's why I'm frustrated. Because I did not start mammograms at 40 and/or because I did not get a mammogram in July when I first reported symptoms to my doctor (albeit vague and difficult to articulate symptyoms), my cancer was caught after I felt a lump in September at age 41. By then it was invasive, agressive, fairly large, and had lymph node involvement (cancer had spread to the lymph nodes). From feeling the lump to being diagnosed took about a month and a half. Treatment began 2.5 months after I felt the lump. With the same timeline, if I'd had a mammograph in July, I might have been diagnosed in September, and started treatment in October.
 |
| retreat and reset |
Would I have still needed chemo, surgery, and radiation? Quite possibly, but my second surgery to take lymph nodes out was a close call. The plastic surgery to repair the lymph drainage system only happened because of the second lymph node surgery. So if I'd started mammograms at 40, or if I'd been referred to have a mammogram in July, I likely would not have needed the second set of two surgeries (or the extra recovery time) and I might not have needed OT. I know (from experiencing it) that the surgery recovery would have been less painful. I likely would have started radiation by now. If my lymph nodes weren't involved, I radiation would be of a shorter duration (though I don't know if my lymph nodes were involved already in July).
 |
| what were we doing? |
This has been my frustration all along with books and resources that say that mammograms are not recommended for folks between 40-45 or 40-50. They only seem to look at the overtreatment as a problem or at the stress of people whose have biopsies that come back negative (arguably unecessary biopsies). On the other side, they only count deaths and they don't account for the extent of treatment for earlier or later cancers!
 |
| the battle ends with the attention spans |
Love cites a "recent analysis" (recent to 2015) on page 155 that found that women between 40 and 50 have "more agressive cancers that are less amenable to screening", meaning that the trade-offs between screening and deaths "averted" are less impressive than the number of deaths averted in the over 50 age range. So maybe this is part of the answer, but it still seems like there's either a gap in the research or in how the results are communicated to women under 50. I will admit that my lack of medical and research knowledge means that I may also be misunderstanding or simply missing something, but I have tried to find it.
My suggestion for a useful clincial study
Later in the book, Dr. Love says that patients can start their own studies (page 288, chapter 11). I love the idea of encouraging doctors to study what matters to me: how much treatment is requred for 40-50 year olds who don't get mammograms, but do find their own cancers versus 40-50 year olds whose cancers are found via mammogram. Do the former have more surgery, more chemo, more radiation, and more recovery time than the latter? Does the type of chemo, surgery or radiation change? Don't just count up who dies; count up the treatments and the intensity of the treatments!

According to Love, in 2015, our "...our government does have guidelines suggesting that every woman over forty be screened" (page 162). This must have changed since 2015, and I think that currently some places suggest 40 and over (SCCA, Mayo Clinic, etc) and others suggest over 45 or over 50. Love suggests that screenings over 40 be "viewed with some skepticism" (and I disagree) because of the reasons mentioned above.
Breast self exams & exams performed by a doctor
Another interesting bit of research has to do with breast self exams. Most women, at least most women my age have probably encountered the breast self exam card in a dorm shower or doctor's office at some point. Apparently these have fallen out of favor (or should have) sometime since I was last in a dorm shower.

The shower card showed how to systematically check for one's own breast for lumps. Love discusses a study where they were taught women how to do the breast self exams well, but the results suggested that those breast self-exams are not a good option. "The breast cancers detected in the instruction group were not diagnosed at a signiicantly earlier stage or smaller size than those in the control group." (Love, page 160). Both groups found cancer, but the systematic breast self exam group also found more stuff that wasn't cancer.
In the control group of this study, and in general, most women found their own cancer just by accident (and because they know what their body should feel like). This was the case with me, though I'm annoyed, as you've probably noticed, that noticing the non-lump changes (itching, discomfort, sensitivity) wasn't enought to get me a referal for a mamogram back in July. Finding the lump by accident in September did get the mammogram train moving.

What is also kind of amazing is that no one (at least according to this book published 7 years ago) has studied whether physical exams done by doctors are useful in detecting cancer! Lots of studies on mammograms, but not on tha doctor doing a preliminary exampm. Also, doctors aren't trained to do these exams anyway! (Love, page 161)
Coordinated care
Something that surprised me in the book is the way Dr. Love suggests that women may need to coordiante their own team of doctors and care for their cancer. She suggests that the surgeon, oncologist, radiation oncologist, and plastic surgeon might not be in communication with each other. This surprised me, as both the medical providers at SCCA (Seattle Cancer Care Alliance) and in Yakima have operated as well-coordinated teams. The Monday after my biopsy, I was called in to O'hana in Yakima to learn the bad news (the "you have cancer" conversation that must suck for everyone and that made me temporarily hate the poor woman who delivered it), be given a thick manual all about breast cancer, and to discuss the next steps.
Aside: At the time I thought that must be the worst job, informing people about their cancer diagnosis, and assumed that that woman met with people all day or every day to have the same conversation over and over again. I've since done the math (well, I've estimated based on very rough educated guesses) and I figure that conversation probably happens more like once a week or a couple times a month, maybe less. It still sucks, but I'm really glad that it isn't happening multiple times every day.
After telling me I have cancer, showing me a model of what size the cancer was, and talking to me about what sorts of things would be scheduled for me right away and who would be in touch, the kind (and not at all hateful woman) explained that on Friday of that same week, a team of doctors would be meeting to discuss my tumor and my treatment plan. Later, when I connected with SCCA, they also had a similar meeting that involved my surgeon, an oncologist, a radiation oncologist, and a pathologist. In Yakima, when I first met with my surgeon, he already knew my history and had already consulted with the team about what would happen first (chemo) and what the plan was for my whole treatment. This kind of coordination made the whole process much easier, and I can't imagine the added stress of somehow trying to manage that coordination as a patient.
 |
| preparing the dining room for new paint |
The other incredible thing about coordination happened between my two surgeries. I was scheduled for a post-op checkup at SCCA one afternoon in late May. The week before, my surgeon had called to tell me that because of the indeterminate results of my sentinel lymph nodes, she would be asking the tumor board (surgeons, radiology, oncology, and pathology) to advise on whether the second lymph node surgery was recommended. But not only was the whole team meeting again to discuss my situation, since I was coming to Seattle for the checkup, it was a good time for a plastic surgery consult for the Lympha procedure. So SCCA put in a rush referral and I got an appointment with plastic surgery at UW for the same day, early in the morning. Not only did that stuff happen fast, but while I was at the plastic surgery consult, SCCA called me (and when I didn't answer because I was talking to the doctor, they called Sean) to say that I could come straight to SCCA after I was done at UW. When we did that, they got us in quickly, hours and hours before our scheduled post-op. And, the post-op with a nurse had magically turned into a pre-op with the surgeon, too.
 |
| fun new hiding spots in the dining room |
I don't know about medical procedures in other parts of the state or country, but in Yakima, that kind of coordination can't even be expected for a routine checkup with a single primary care provider. My husband and I have both sat in waiting rooms for 45 minutes to an hour (after arriving on time), waiting for our primary care doctor to see us, only to sit for an additional 30 minutes in an empty exam room. (And if you are tempted to suggest we switch doctors, know that I can easily count 4 different providers/clinics where this has happened.)
 |
| the cats needed a dinner escort to help them eat after we moved their food dishes out of the dining room |
I don't know if the tumor boards and coordinated meetings of providers are new since 2015, regional (though I know my nephew has had a similar experience), or a lucky coincidence for me, but I'm glad that this section of the book bore little resemblance to my experience.
 |
The new dining table location, near the lego city means a new diner table conversation topic (and a cat hiding spot)
|
Tumor Margins
I was surprised to read about how clear margins are actually determined, according to Dr. Love. When they took out my tumor (and my nephew's), I was under the impression that they sliced the whole thing up and checked for cancer cells all the way around the surface of the mass they removed. According to this book, They take a slice (or several) out of the lump and check the margins of the slice, but they don't check the entire tumor. This means that when they find clear margins, the haven't checked absolutely everything. It also means that they might accept a few isolated tumor cells at the margin, as long as the main mass of the tumor wasn't at or across that edge.
 |
| Cali, asleep on the lego sorting job |
This makes sense, once you think about it, but wasn't what I imagined. However, it does help me understand why they need to do more radiation in that area. In my case there will be both radiation to the whole breast and lymph node area as well as a "boost" of radiation at the hole (my phrasing not theirs) where they cut out the tumor. With this definition of "clear margins" instead of an absolutely certaintly that no cancer cells could possibly be in that area, radiation makes sense (or in doctor speak: "is indicated").
Order of Treatment
The book was generally a little disorienting to read for two reasons. First, though the author acknowledges that chemo may be the first step in treatment, the assumption often seems to be that chemo comes last. As a result, with my chemo coming first and surgery second, I sometimes find myself a little lost. Do my lymph nodes count as having no cancer (now) or do they count as being "involved" (as they were originally) because I am partway through treatment?
Similarily, was my tumor 2.3 cm (roughtly the size it was on biopsy), 4.5cm (the side it was in an MRI three days after chemo had started) or 1.2 cm (the size it was after chemo when it was removed)? Ultimately, it probably doesn't matter, but I don't know how to orient myself with statements like
"Also the mere presense of cancer cells in a lymph nodes is no cause for alarm. Lymph nodes that contain single isolated tumor cells or small clumps of tumors cells, so called micrometastates, may not signify any worse behavior than if they are completely negative" (Love, 216).
Because my chemo came first, this statement doesn't apply to the status of my tumors after surgery. My surgeon and the tumor board determined that the isolated tumor cells in my lymph nodes were cause for concern because they were still there after chemo, which is why I had the second lymph node surgery. It's not a big deal, but it is disorienting for someone who did things out of the "standard" order, even though the author acknowledges, earlier, that either chemo first or chemo later could be the standard order.
 |
| Cali, being attacked during lego sorting |
I was also bothered by the way that the author would sometimes put in personal anecdotes or itnerpretations that didn't seem to match the studies she had just cited. I appreciated both her inclusion of the studies and her discussion of the studies' shortcomings, but she'd sometimes toss off something that just didn't seem to fit, either her interpretation or an anecdote that didn't match the study results.
 |
| Buddy being snuggly upstairs |
In the section on chemotherapy, they mentioned that Adriamycin, one of the chemos I had, can cause heart problems for "...about one in two hundreed treated women." But then goes on to say that "One of my former patients developed heart disease...and ended up with a heart transplant." It's rare, based on the statistic, but then it's terrifying based on the anecdote!
 |
| asking for head scratches |
I also found that the discussions of the relatively agressiveness of tumors with different markers was confusing, since I think it means had a more agressive form of a less agressive tumor. Tumors can be judged by size, how fast they appear to be growing (which, at the outset is judged based on how the cells from the biopsy look, not by waiting to see how much the tumor grows), and based on whether the tumor reacts to hormonse (ER+) or HER-2 overexpression. On the first test, my tumor was inconclusive for HER-2, but the second test showed that it was HER-2 negative. However, Love says that "Almost all DCIS is HER-2/neu positive..." (page 219). Which makes me wonder if my DCIS, which was identified and removed during my lumpectomy, means that overall I was both HER2- and HER2+.
 |
| Alison is teaching him to jump up for head scratches |
My tumor was ER+ and HER2- and it also had a Nottingham grade of 9/9 (high grade), meaning it looked like it would grow fast. My doctors did not do this special test to determine the Ki-67 protein level, because my ongologist said they already knew it looked like a fast growing cancer. I can't tell if the Ki-67 is something that was done in 2015 and isn't done now or if it's use is a local or situational decision. I believe this means that my cancer was Luminal B, but I'm not entirely sure if I ever got a clear identification of whether my "recurrence score" was high or low. Discussions in online breast cancer groups seem to indicate that lots of people get an oncotype test, but I didn't. I believe the oncotype test tells the recurrence score, but I'm not entirely sure what that means or why I didn't get it. Or maybe I get it later.
Aside: Many sources and individuals refer to "early stage" cancer, but I'm never quite sure if I qualify or not, before or after chemo. Similarly, individual well-wishers tend to say "I'm so glad they caught it early" despite having no idea if they did, indeed catch it early.
As far as I understood from my doctors, The ER+ was good news, because they could fight the cancer with hormones. The HER2- meant that they couldn't fight it with Herceptin, and the indicators that it was fast growing were, of course, not great news. This book suggestes that most tumors are Luminal A and most of the hormone risk factors (including use of birth control, late pregnancy, and hormone replacement therapy) are predictors of this kind (page 221). As the only risk factor I can identify for myself is birth control (and my doctor bluntly said that my birth control didn't cause this cancer), and I think I have Luminal B, I'm right back to (what my doctors said at the start) no clear risk factors or cause.
 |
| training |
However, some things do seem to match my experience. On page 224, Love says, of ER+ tumors "...the ones with a higher reurrrence score had both a higher rate of recurrence and a better response to chemotherapy, suggesting that the biology of the tumor is more important at predicting prognosis and the best treatement than the stage of the cancer." My tumor did have a good response to chemo, which unfortunately makes me think that means the risk of recurrence is high, too.
In the Recurrence section of Chapter 17, Love indicates that ER+ cancers (like mine) "have their [peak rate of recurrence] at four years" (page 465). This means I'm tempted to put a celebration date for, say, September 2026 or 2027 in my calendar. I don't yet have my radiation dates scheduled, but I'm still thinking (hoping) that I'll be done by the end of August or September this year. Which, incredibly, means that I will have been "dealing with" this darn thing for basically a full year from when I first felt the lump. Today, as I write this, I am essentially one year out from when I started noticing symptoms. Sigh.
Testing & Scans
Love says that imaging isn't useful for finding bits of cancer that may have spread to other parts of the body, "So we don't do those tests now unless we have a reason to think the cancer is likely to have spread because it is large or agressive or because you have worrisome symptoms such as a cough or weight loss" (page 233). She goes on to say "The exception to this is when we are going to give chemotherapy first and surgery second and you have symptoms..." This seems to contradict my experience, as I didn't have symptoms. I did have scans done before my chemo began. I believe the size of my cancer wasn't understood to be "large" even though it was larger in December than it was in May. To add to my confusion, a few pages later, on page 235, she says that medium size tumors with lymph node involvement will get bone scans and CTs (like I did).
 |
| watch that foot |
The book also suggests that I shouldn't have gotten an MRI ahead of time unless I had extrememly dense breasts, was being considered for a different type of radiation (XRT), or if I needed a breast reduction (page 247), but I did have an MRI. The book says an MRI means a risk of finding more suspicious stuff that might lead to the recommendation for a mastectomy, but my doctors wanted an MRI to more accurately identify the size and location of the lump for later lumpectomy. My reaction is that the tumor was a lot larger when I got the MRI than when I got the earlier scans and biopsy, so I'm frankly glad to know that the chemo reduced the size from 4.5 cm to 1.2 cm, rather than from 2.3 down just about 1 cm.
Radiation
Reading the section on Radiation was helpful because I haven't started that yet and there were a couple of questions I now have for my doctor. However, mostly the doctor had already explained the important parts. There are some really terrifying options for radiation with a balloon in the breast or these horrifying looking rods inside the breast that can have radioactive things inside them. I skimmed these sections, horrified by the diagrams, and happy that I didn't have to understand them fully.
 |
| and those claws! |
The funny (to me) addendum to this was the phone call I got for scheduling Physical Therapy. My Occupational Therapist referred me to a Physical Therapist at the same place to help me ease back into exercise during radiation (she seems to think that without a PT guiding me, I'll overdo it). When the PT scheduler called, I mentioned that my schedule for radiation was as of yet undertermined, at which point she said the Physical Therapist she was scheduling for was pregnant, so I couldn't meet with her if I was doing radiation. There was a long pause, at which point I remember FAQs for radiation telling me that I wouldn't be radioactive. I told the scheduler this, but she wouldn't take my word for it and wanted to wait to consult with the PT person.
My mom asked a good question the other day: Why does radiation kill cancer but doesn't damage the lymph nodes. The book didn't explicitly address this, but it seems to be that radiation kills all cells, but the lumph node cells are able to grow back because they're supposed to be there or because they are fundamentally healthy. I suppose there are more node cells in a lymph node than cancer cells, so many that's it.
 |
| and back to cuddle |
Surgery, ALND, Reverse Axillary Lymphatic Mapping
In the surgery section, chapter 13, the author describes an alternate treatement (reverse axillary lymphatic mapping) for reducing the risk of lymphedema with an Axial Lymph Node Dissection (ALND). The arm is injected with blue dye that highlights the lymph nodes that drain lymphatic fluid from the arm so the doctor can avoid removing those. The idea is that avoiding those lymph nodes would prevent lymphedema in the arm and presumably the breast wouldn't be draining cancer cells to those lymph nodes anyway (page 345-6).
My surgeon mentioned something about dye and massage of the arm before surgery but didn't explain because I opted for the Lympha plastic surgery instead. My arm was blue when I woke up, so maybe they did this, but I'm not sure.
 |
| this guy used to be feral, but he is so friendly now |
Apparently the lymph node biopsy and dissection can both result in pain, numbness, or tenderness in the area even five years later (page 348). This looks like a question for the lymphadema clinic folks, but I didn't ask because there was a lot going on. I'm signed up for something like 7 more visits, so I've probably got time. It did sound like the numbness, at least, might last quite a while. In the last two weeks, the pain has gone from a daily annoyance to an occassional twinge, mostly due to activity (or, perhaps more accurately, due to too much activity).
Hair Loss & Premature Menopause
I was a litte surprised to read that "...in most women the eyelashed and eyebrows only thin a bit" (page 435), since I lost my eyelashes entirely and it was super weird! All the hair is coming back now, though at slightly different rates. My eye lashes are fully back, but I don't remember the tips being blond/white. My head hair is really short, and more white than it was last time we met, but I'm happy that the front is filling out.
 |
| check out that hairline on the top! |
According to Love, "60 percent of those over forty will become menopausal [after 4 cycles of AC chemotherapy]" (page 424). It sounds like it may or may not be permanent. The two biggest symptoms I've noticed, are that the skin on my face cleared up (is that the fault of chemo or menopause or both?) and that I have hot flashes. The hot flashes appear to happen randomly, though Love advises me to "avoid triggers" like "spicy foods, caffeine, stressful situations, and hot drinks..." (page 491) to which I say: reading that suggestion was a "stressful situation." I can't tell what triggers the hot flashes, since they seem to occur regularly when I'm sitting calmly on the couch in the evening and when I go to bed, but also randomly during the day. Since reading this, I've tried to gauge whether food/drink might be related, but I can't identify the link (they don't happen close enough in time).
 |
| twins |
In another of her frustrating anecdotes, Love explains that after her cancer treatment (unknown treatment for a different type of cancer) she only had hot flashes for 10.5 weeks and then her period came back and she was done with the temporary menopause. I found this pretty annoying, since her situation has basically no bearing on mine or on breast cancer patients generally. It's another anecdote that doesn't really illuminate the experience of breast cancer treatment.
Conclusion
It seems like I should have a conclusion, after all this writing. The book is good, but out of date. It's hard to tell which bits are, in fact out of date, so in all cases where my doctors' advice directly contradicts the book, I figure I can trust my doctors to know the latest and best information. And, of course, I've already followed most of their advice, etc before reading this book.
I did, however, find the depth of the explanations on a number of topics to be helpful and because it's a big 'ol book, the author was able to give more depth and more explanation than my doctors could.
I think the simplest take-away is that it is unfortunate that there wasn't a more recent edition that I could have read, but I'm glad I was able to read this one.