I have now completed the first full week + two days of my radiation therapy. Last Wednesday (earlier than I had expected it could happen), I had kind of a practice run, and then real radiation treatments on Thursday and Friday. This week I've had five more treatments. I have radiation daily, M-F, through the start of September. I've got six and a half weeks total, or 33 treatments. The radiation is targeting the whole breast as well as the lymph nodes in my armpit and those near my collarbone on the left side. The last week of treatments will be a boost to the area where they removed the tumor lump from my breast.
 |
| some bulbs I've nearly finished, underglazed and now waiting for glaze |
Why my treatment has to be so long
I had some trouble, and apparently keep having a bit of trouble, understanding why the treatment has to last so long. I'd read about accelerated whole breast radiation (or hypofractionated radiation therapy for breast cancer) and couldn't understand why "new guidelines" from 2018 for speeding up treatment wouldn't apply to me. I asked my doctor last week why my treatment couldn't be sped up. She explained that my treatment couldn't be accellerated because I'd already had chemotherapy, which pacified me for a week until I started to write this post and fell down the same rabbit hole, again, when I saw the bullet list from the BreastCancer.org article that says "The decision to offer hypofractionated whole-breast irradiation should not depend on...previous chemotherapy." I reread the PubMed article (I've read a whole lot more medical research reports this year than ever before in my life!) and did, eventually figure out that my issue is the combination of lymph nodes and previous chemo.
 |
| a detail of the underglazing process of a sculpture I'm working on |
Not only is there a lot of dense information out there, and not only does breast cancer have a lot of complications and variables (hormone status, HERS2 status, nodes, size, and grade), but when I read about it, I'm not an unbiased reader. Especially in this case, I wanted to find that my treatment could be done more quickly, so I had trouble finding or understanding why it couldn't.
 |
| the sculpture with the orange underglaze layer partly removed |
As my doctor originally, said, and as I finally accepted (twice), because I've already had chemotherapy, a systemic treatment that impacts the whole body, not just the breast, the increased dose of accelerated radiation risks causing scar tissue to my lymph nodes. If the cancer had never been in the lymph nodes and I'd had chemo, I could have tolerated the increased dose of radiation to just the breast that is delivered in the accelerated approach. The unspoken part of this, too, is that my lymph system is already working at a deficit because I'm missing 15 or 16 nodes (because they were removed).
 |
| the orange underglaze removed, ready for glaze |
Radiation & preparation
Wednesday's practice was longer than the actual treatments, as they were checking that everything worked right, I think. The pillow thing ("cradle") they made for my arms was apparently unusually wide, as they had to kind of break off part of it to get the machine to fit on the right side. (When I walked into the room for the practice, one of the radiation techs who hadn't met me before said she was surprised I was so small given the size of the cradle). They also changed the position of my right arm from what it had been during the planning CT scan. That means that my right arm doesn't go into the molded position of the pillow. It also means that every few days, when a new person is working in the radiation room, they will tell me that my arm is in the wrong spot. I suspect it may contribute to the feeling of loosing blood flow to the fingers of my right hand.
 |
| bulbs in the kiln with the first underglaze layer or waiting for their first bisque firing |
The radiation itself is pretty quick. I walk into Northstar, tell the person at the front desk (who usually already knows my name) that I don't have COVID symptoms, then walk directly into the changing area and grab a gown. The gowns are sized for people who are much taller and much larger than I am. It's unfortunate, because with how warm it has been, I don't really want extra fabric on my body, luckily they let me leave my shorts on, so I can just leave the gown wide open in back for a pleasant breeze.
 |
| I thought the gown was big on me, but then a smaller woman walked in and hers just about dragged on the floor! |
Depending how early I get there, I wait next to the changing rooms for anywere from 1-10 minutes (though, honestly, the first day was the longest wait and usually if I show up early, they get me in early). Then a radiation tech comes to take me back to one of two radiation rooms. Since they make me take off my watch when I change, I'm not sure exactly how long the whole process takes, but I timed the process from watch off to watch on again after I get dressed and that was 12 minutes. In the radiation room, I lay down on the bed thing, get my arms and head positioned in the pillow depressions and the techs running the machine put a lift under my knees and a foam foot holder in place (presumably to keep me still and in the same position each time). Usually the knee holder is slightly sideways--I assume this so that I don't get too comfortable.
 |
| The cradle thing that positions my arms looks more like the "inferior vaccum bag form" on the right, though it isn't blue. Image from Smither's Medical Products. |
Next they check the tattoo(s) on my side to make sure I'm positioned right. They've only adjusted me twice, which worried me at first, since it seemed too easy. They position me using a couple of laser lines. I can see myself in the reflective glaze in the ceiling and also in the reflective part of the radiation machine. From above, the lasers form a green + across my chest and left arm and up the side of my body. They cross near my shoulder. From the side view of the reflective glass in the machine, the one laser line follows the countour of the breast being treated.
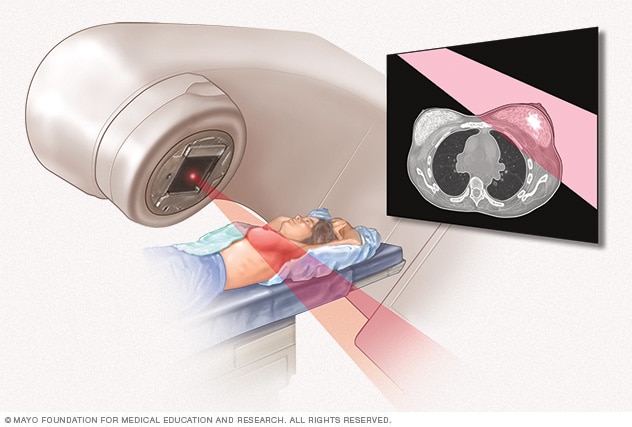 |
| This diagram form the Mayo Clinic shows what's happening in the machine, and also gives a pretty good approximation of how I'm positioned |
After checking my position based on the tattoo on my side, they have me take a breath and hold it so they can check the tattoo near my shoulder. They rub the bottom of a block thing (to warm it up, I think) that looks like an alarm clock and put it on middle just below my breasts. This block somehow tells them if I've taken and held my breath correctly. Someone says "twelve point nine" and part of the radiation machine whirrs itself over to my right side where it almost touches my elbow. This is the part where they needed to hack away part of the pillow during the practice session last Wednesday.
 |
| This picture is similar to what I experience, and shows the round part tilted to the side. I found the image on RadiationInfo.org |
Every day except for the second Thursday, the sequence has been the same. They say that we are ready to start and the techs exit the room. Then someone on the intercom tells me to take a breath and hold it. The machine whirrs a bit, then stops and the tech tells me to breath. Both the bed and the other parts of the machine can move. When we start, the biggest part of the machine, a round white part roughly two and a half feet wide is looming over me at about a 45 degree angle, nearly touching my elbow and the cradle. This has a ten inch piece of glass (that I can see my body and the laser reflected in) with metal teeth things behind it. The teeth are long metal pieces with pointed ends that can open and close all together or separately. I looked it up, and this is called a collimator. As I had guessed based on watching it in action, it is used to control the shape (and size) of the radiation beam.
 |
| The collimators on the machines I use look a lot newer and more friendly than this picture from the cyclotron at University of Washington (image from Wikipedia) |
Next the metal teeth-looking parts of the machine close most of the way. The teeth are behind glass and can all move together or move independently. That part of the machine starts on my right, very close to my body and face. The first breath hold is in that position and lasts about 10 seconds. Next the teeth move, then the collimator moves to be directly above me. The short breath hold is followed by two long breath holds each lasting about 20-25 seconds (as measured by my highly inconsistent counting methods). The collimator moves to my left and I don't know what it does over there because I'm required to look to the right the whole time and my reflective surface doesn't extend that far. I have another short breath hold with the machine on that side. Then it's all over, but I have to wait for the techs to lower the bed thing which has raised up while I've been prone.
How I'm handling it
After the first few times, I was worried, actually, that it was so easy. They've only corrected my breathing once (told me to let a bit of air out) and they've only adjusted my position twice. It felt too unlikely that I got myself into the exact right position on the first time every day. But I've now met with my radiation oncologist twice (last Friday and this Thursday) and she said that I was doing great with my breath hold (yes, I was complemented by a professional on my ability to breathe).
Thursday I was mildly alarmed that the order of the machine's movements and the timing of my long and short breath holds was different. The technicians explained that at the end of each week they'd do something a bit different. I didn't understand it, but I was mostly just checking for them to say "oh no! we gave you somebody else's radiation today" or something, so I was happy when that didn't happen.
So far I don't appear to be having a skin reaction to the radiation. Everything I've read or been told by folks who've done radiation makes me think my best shot at avoiding a painful skin reaction and/or the fatigue that many people complain about is to apply lotion to the area every day, wear loose clothing that doesn't rub or constrict the area, drink plenty of water, and exercise. The nurse and doctor both said that they can't really predict if I'll have a bad reaction, but suggested those same things to try to prevent it. Apparently being on the smaller side is a potential advantage, as more breast tissue can mean a worse reaction. On the other hand, it sounds like pale and/or sensitive skin might also mean a worse reaction, so I'll just have to wait and see. Women who've had radiation say that the reaction is worse the longer the treatment goes, and mine is longer than most I've heard of.
I'm presenting all this calmly now, but last week I was nearly in tears from how worried and generally stressed out I was about starting radiation. I was disappointed that the 5-6 weeks of radiation predicted in December had become 6.5 weeks. I hadn't realized how much I was counting on more time between radiation and the start of the Fall quarter at YVC. Northstar got me in faster than I thought they'd be able to last time I posted, but the extra surgery and the recovery time after surgery extended the timeline beyond what I'd been hoping back in December or April.
As it stands, I will be finishing radiation on September 6 (my previous estimate ws that September 7 was the earliest time possible, and I'd forgotten about the holiday). Convocation for faculty and staff at YVC starts the next week (with students returning the week after). I'm doing everything in my power to set myself up to be not fatigued (exercise) and not in pain (lotion and hydration) in the last weeks of radiation and the time right after, but I've had some setbacks on the exercise side of things. The last weeks of radiation and the weeks right after are when others tell me they had the hardest time. Worrying won't help, and I can't change the weather, so I'm trying to keep my focus on what I can do today.
 |
| interior view of my studio during the 2021 Tour of Artists' Studios |
Tour of Artists' Studios over Labor Day weekend
With the assumption that I'd probably be done with radiation by then, I agreed (months ago) to have my studio on the Yakima Artists' Studio Tour over Labor Day weekend. I did this last year and I like the idea of the tour coming to my house, rather than having to bring myself somewhere else. My colleagues and friends, Chris Otten (photography instructor at YVC) and Monika Lemmon (painter, mixed media artist, and soon to be drawing instructor at YVC) will also be at my house and I've told them if I feel bad they're in charge of all the hard stuff.
 |
| sign from last year's Tour |
If you would like to visit me on Labor Day, my studio will be open Saturday and Sunday from 10-4 and Monday from 10-12. Tickets are $10 each and you can purchase them from me ahead of time or when you get to the studio. You can also buy them from other artists and locations, but I make more money if you buy them from me. I am hoping to have some of my new port-a-cath mugs and bulbs and sculpture done before the show (and some bowls, too, if I really get motivated), but my studio time has been unpredictable this year and this summer.
 |
| port-a-cath and heart-a-cath mugs waiting for glaze |
Physical Therapy & a little set back
I also started Physical Therapy (PT) this week, in addition to continuing my Occupational Therapy (OT). The OT (at the lymphedema clinic) is mostly focused on increasing my range of motion and preparing me for how to prevent lymphedema, as well as how to recognize the symptoms of lymphedema. I've learned and have been doing some exercises to increase range of motion in the left arm (after they cut into it and removed a bunch of lymph nodes). I've also learned and have been practicing lymphatic drain massage, which is intended to "prime" the lymphatic system and help drain lymphatic fluid away from the arm and the side of the body where the surgery was and the radiation continues to be. Radiation is (hopefully) the most taxing thing that's going to happen to the weakened lymph system on that side. |
| the cats know it is too hot |
The PT is also focused on increasing range of motion, as well as increasing strength. The exercises she has me doing involve a bit more of my body, with the idea that other muscles in the back, trunk and shoulder support the arm. My physical therapist also talked with me about how to adjust my position so that I don't get backaches while typing on the comptuer for a long time. My goal is to get back to regular exercise and weight lifting, but this week I had to readjust my ideas of how fast that might happen.
I have radiation every day and was scheduled for OT and PT on Tuesday, but OT called and said that those three things in one day were too much, especially in combination with the high temperatures this week (highs have been 107-110 this week). So I did PT and no OT that day. PT Tuesday was mostly first-day kinds of stuff, like getting my history and checking my range of motion and posture. At this point, the history of my medical experience this year takes some time to relate. We also did a few exercises and she gave me some homework stretches.
 |
| We don't have AC or insulation upstairs, so the cats intentionally choose the hottest spots in the house |
That night, Tuesday, I walked down to Davis at the end of Alison's band practice with the idea that I'd walk home with her. It was 9pm, but still 91 degrees out. I only walked two blocks, but they were late getting ou. Basically I was out in 91 degrees, no sun, for 10 minutes, including a casual walk (downhill) and standing around. But the heat bothered me so much that after 5 minutes of waiting, I started back home. My OT had told me to watch out for being outside in very hot weather for too long. I think she said above 103 for 15 minutes. This wasn't that, but I still got scared. My husband happened to be driving home right then, so he actually picked up up a block from home and drove me home!
 |
| melty warm stretches |
My OT said that I could do up to 20 minutes of exercise every other day, but I needed to keep it low impact and I couldn't use weights. So Wednesday morning, following her instructions, I did a (modified) 20 minute indoor cardio workout video which seemed fairly mild compared to what I used to do. It didn't seem like a strain, but by the end of the day Wedesnday, the side of my chest under my arm had swelled a bit. It isn't clear whether the swelling was from the heat or the exercise (or the radiation), but when I saw her on Thursday, my PT suggested I reduce my activity to just 10 minutes every other day.
It feels very strange to do so little, especially as I've been advised that I should be exercising during radiation to ward off the fatigue. This week, there really isn't anytime when I can walk outside, let alone run (or jog). Last week I was avoiding walking between 10am and 5pm, but this week even getting up at 7am or walking after 9pm didn't work, since it never gets cool enough during that time. Maybe I could walk in the middle of the night, but I'm not sure that's a great choice in my neighborhood. Instead I've been driving to Target or Lowe's to walk inside.
 |
| the weather on Tuesday night at 9pm (91 degrees), and forecast for the week (108 on Wednesday, 110 on Thursday and Friday) |
I went back for a second PT appointment on Thursday and we did more than on Tuesday, though my idea of what I "should" be able to do by now and My PT's idea of what I actually "should" be doing right now to ease myself back into my previous routine are not perfectly simpatico. She started me on an exercise machine that was a bit like a recumbent bike. There was a place for my feet and bars for my hands, though she didn't want me to use my feet. The wildest thing, to me, was that she turned the seat 90 degrees to the side, then had me sit, then turned it back to front-facing before I began. She had me gently use my arms to pump back and forth for about 2 minutes, then she turned the seat to the side again before I got up. Meanwhile, I'm thinking that last time I was on a similar machine, I did 20 minutes of intense rowing! Of course, that was way back before Covid when I used to go to the Y (without a mask).
 |
| I feel like I've been assigned the cat-level of exercise |
After the rowing, we did a variety of arm exercises, while my PT corrected my positioning. I tend to arch my back backwards to get my arm up higher and I tend to lift the left shoulder. She says this is normal in folks who've had a surgery like this, as we instinctually do that to protect the shoulder. The challenge is to work against that instinct, while increasing strength and range of motion.
 |
| Another sculpture I'm hoping to have finished for the Labor Day Tour |
Of course the other challenge is to be patient with the process. I still have some swelling today (three days after I first noticed it), though I've been avoiding the heat and continuing to do the lymphatic massage. It doesn't appear to be worse, but I think I'll feel better once I see my OT on Tuesday. I anticipate that I'll be gently scolded for overdoing it, but I'm hoping she'll also be able to give me a sense of how concerned I should be and if there's anything else I can do to make it reduce. The PT, on Tuesday and Thursday was very good at helping me understand better the parameters of what I am and am not allowed to do, which I appreciate very much, even if it is annoying to have these restrictions.






No comments:
Post a Comment
Tell me what you think about my work or this post